Herpes
Coping and Support
Helping Others Stay Safe
People with the herpes virus must take precautions to avoid spreading the virus to other people. During active outbreaks, people should keep affected areas away from other people until the symptoms have healed.
These steps are particularly important with genital herpes. Because genital herpes can be transmitted during and between outbreaks, patients should:
- Have their partner(s) undergo blood tests to determine if they have antibodies to the virus. Knowledge of a partner’s status helps couples to decide what steps are required to reduce the risk of transmission.
- Consider abstaining from sex or practise mutual monogamy with one uninfected partner.
Pregnant woman with genital herpes and who have active symptoms can transmit the virus to the baby as it passes through the birth canal. To prevent this, birth by Caesarian section is recommended. A doctor will advise the mother on the best form of delivery.
People with oral herpes must also take precautions:
- Never touch an open sore and then your eye, as it can result in herpes keratitis.
- Avoid touching a newborn baby, as newborns can be infected by exposure to HSV.
- Use condoms or other barriers during oral sex to reduce the risk of transmission.
People with herpes zoster will also need to be cautious. Shingles itself isn’t contagious, but the virus that causes it can be spread from a person with active shingles to a person who has never had chickenpox during the blister phase through direct contact with the rash. The person exposed would develop chickenpox, not shingles.
- The contagious phase is from blister onset to blister crusting.
- The virus is not spread through sneezing, coughing or casual contact.
- Somebody with post-herpetic neuralgia is not infectious.
The best thing to do is to lower the risk of contagion by covering the rash. Don’t touch or scratch the rash, and wash your hands often. Once the rash has developed crusts, you are no longer contagious.
During inactive periods, symptoms may not be present, but viruses may still be shed. With genital herpes, people should:
- Use latex condoms to protect the mucous membranes that are the most likely sites of transmission. Note that condoms do not cover all the potential sites for shedding (i.e., nearby genital skin).
- Consider undergoing daily suppressive therapy using valacyclovir, which has been shown to reduce the risk of herpes transmission.
- Develop good hygiene habits. The virus may be transmitted if the skin in uninfected areas is touched after contact with an open sore.
Psychological Care
The psychological stress of having herpes can vary depending on the type of virus a person has. For example, common reactions to a diagnosis of genital herpes (and its association as a sexually transmitted disease) include shame, depression or anger. These emotions often fade over time. In addition, some people may find it hard to adjust their sexual habits and lifestyle to prevent spreading genital herpes. For people experiencing emotional distress after a diagnosis, seeking professional support can help them to:
- Recognize that a genital herpes infection is a health issue, not a moral judgment.
- Develop a positive self-image and stop perceiving genital herpes as social stigma.
- Stop assuming that having herpes will prevent them from being romantically involved or having successful long-term relationships.
Professional counselling may also benefit people with herpes zoster if they are distressed over physical symptoms, lifestyle changes, or their personal appearance.
Physical Care
The physical impact of herpes on infected, otherwise healthy individuals is the pain and unsightly appearance of the blisters during outbreaks. The pain can be mild, as in the case of a minor oral herpes outbreak, to severe, as in the case of shingles.
People with herpes zostercan be intensely uncomfortable. Some people with shingles also develop post-herpetic neuralgia, a long-lasting pain that persists long after the rash has subsided. This pain can be severe enough to cause insomnia, weight loss, depression and preoccupation with finding pain relief. Both shingles and post-herpetic neuralgia can disrupt daily activities. Some people experience extreme sensitivity and find gentle touches, drafts and temperature changes unbearable. For these reasons, people with herpes zoster will want to work closely with a doctor to manage and alleviate their condition.
Regardless of the type of herpes virus a person has, pain and discomfort is best managed with the help of your doctor.
Overview: What is herpes?
The information in this section has been gathered from existing peer-reviewed and other literature and has been reviewed by expert dermatologists on the CSPA Medical Advisory Board.
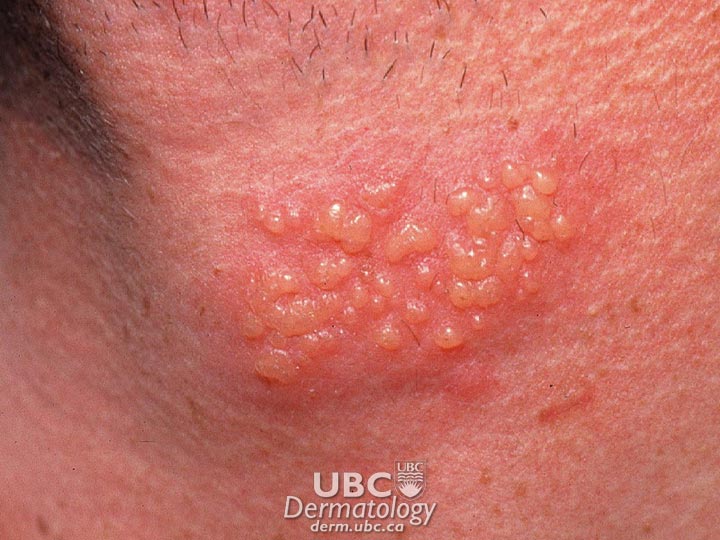
Herpes is a common viral infection that causes uncomfortable blisters on the skin and mucosa. In 50 per cent of cases it lies dormant indefinitely in the body’s nerve cells, where it can later reactivate and cause further blisters. There are two main types of herpes virus: herpes simplex and herpes zoster.
Herpes simplex is the cause of oral and genital herpes, and herpes zoster results in chickenpox and shingles.
The herpes simplex virus (HSV) can be further divided into two types: Type 1 (HSV-1) and Type 2 (HSV-2). HSV-1 is most often responsible for cases of oral herpes, and HSV-2 is most commonly responsible for cases of genital herpes. However, HSV-1 can infect the genital area.
Both HSV types are characterized by the same pattern of infection. The primary infection occurs when the virus first infects an individual. In about 10 per cent of cases, sores or blisters develop. In others, there may be mild or no visible symptoms. The itchy, painful blisters break and form sores that eventually heal. The virus, however, remains in the body.
After a latent period during which the virus remains inactive, patients generally experience several subsequent infections a year. Over time, the severity and frequency of these recurrent infections decrease. Recurrent infections may be triggered by various factors, including fever, stress, excess sun exposure, trauma, or a menstrual period. They may also recur for no obvious reason.
 herpes simplex-1
herpes simplex-1  herpes simplex-2
herpes simplex-2
Herpes zoster is an acute, localized infection caused by the varicella-zoster virus, the same virus that causes chicken pox. After a chicken pox infection, the virus remains in some of the body’s nerve cells where it lies dormant (inactive) until reactivated. The reactivated virus travels along nerve fibres toward the skin, multiplies, and causes a painful, blistering rash known as shingles. Very rarely, shingles can lead to pneumonia, hearing problems, blindness, brain inflammation (encephalitis) or death. In some cases (usually in the elderly), a painful condition called post-herpetic neuralgia (chronic pain) persists after zoster disappears and can last for many months afterward.
Herpes is not dangerous in otherwise healthy individuals; however, the sores (if present) may be painful. In immunocompromised individuals and newborn babies, herpes can be serious but rarely fatal. Unfortunately, the virus may be spread even when there are no symptoms (asymptomatic shedding). Many infected individuals are not even aware they carry the virus.
Symptoms
During the primary infection of oral herpes, these symptoms may occur:
- Small fluid blisters appearing on or inside the mouth or on the back of the throat
- Swelling of the lymph nodes in the neck
Symptoms may be mild or go unnoticed. Subtle symptoms may be mistaken for small cuts, bites or pimples.
In recurrent infections:
- When symptoms occur, they may appear as blisters or sores that generally heal more quickly than primary infection lesions.
- Many patients experience warning symptoms such as itching, tingling or pain 1-2 days before recurrences.
During the primary infection of genital herpes, these symptoms may occur:
- Some people develop one or two crops of sores or blisters within days, but sometimes within weeks or months of infection.
- Sores/blisters may appear on the penis or vulva, near the anus, or on the thigh and buttocks.
- Sores and blisters may break, ooze fluid, crust over, and heal in 2-4 weeks.
- Fever and swelling of the lymph nodes near the groin may occur.
- Headache and painful urination may be experienced.
- Some people develop minor or no symptoms.
These effects may appear in recurrent infections:
- Symptoms may appear as blisters or sores.
- Many patients experience warning symptoms such as itching, tingling or pain 1-2 days before recurrences.
{jkefel title=[Looking Deeper]}
In both HSV Type 1 and Type 2 cases, the infection follows the same course of action. During the primary infection, the virus makes multiple copies of itself, which mobilizes the body’s defences to fight the virus, thus limiting its spread. The defensive action may result in the characteristic sores and blisters or it may result in no visible symptoms. If present, the itchy, painful blisters break and form sores that eventually heal. The virus then retreats from the skin along nerve pathways to nerve cells where it establishes a small, permanent colony. During this resting phase (latency), the virus does not trigger the body’s defences. During the recurrent infection, the virus is reactivated, causing it to travel back down nerve pathways to the skin, where it triggers a recurrent infection. The virus again begins to multiply. This recurrent infection may result in sores and blisters similar to the ones exhibited during the primary infection; alternatively, there may be no symptoms.
{/jkefelend}
For both oral and genital herpes, transmission is by skin-to-skin contact when the virus is active. The virus is transmitted when a contagious area (lesion) comes into contact with breaks in the skin or mucous membrane tissue, usually in the mouth and genitals. The virus cannot breach intact skin.
- Most cases of oral herpes are transmitted during childhood by infected persons kissing or sharing eating utensils or towels with family and close friends.
- Most cases of genital herpes are transmitted during sexual contact with an infected person. It is possible for a person to contract genital herpes from oral sex with a partner with oral herpes.
- Both oral and genital herpes can be transmitted whether symptoms are present or not.
- Mothers can transmit genital herpes to their children during childbirth.
Herpes zoster is caused by reactivation of the varicella-zoster virus after a chickenpox infection. It is not clear what reactivates the virus, but a weakened immune system (which helps fight infection) may cause the virus to move along nerve fibres toward the skin where it multiplies and causes the symptoms to appear. Illness, trauma and stress may also be triggers that reactivate the virus.
If blisters break, the virus can be transmitted by direct skin contact to somebody who has never had chickenpox. That person will develop chickenpox, not shingles (although shingles can then occur later in life).
The herpes zoster virus typically results in the following symptoms:
- Reddish rash that turns into groups of blisters within a few days. Blisters crust and heal in 2-3 weeks. Most commonly, shingles occurs in a single area on one side of the body, in a strip or band of skin supplied by fibres from one nerve. This may show up as a banded rash wrapping one side of the trunk from spine to sternum.
- Burning, tingling pain, or skin sensitivity in one area on one side of the body. Pain may begin a few days before the rash and can range from mild to intense.
- Possible headache, fever, chills, nausea, diarrhea.
Complications following a diagnosis of herpes zoster include:
- Post-herpetic neuralgia (chronic pain). In about 1 in 5 cases, severe pain persists for months to years after the rash disappears. Elderly patients have a higher risk of developing post-herpetic neuralgia. Most people with post-herpetic neuralgia get better with time, usually within a year. A few people develop chronic, persistent pain.
- Herpes zoster ophthalmicus. Shingles of the eye causes swollen eyelids, eye redness and pain. Without prompt treatment, this can scar the eye, cause vision damage or lead to glaucoma, which can cause blindness.
- Ramsay Hunt Syndrome occurs when facial nerves are involved and includes facial paralysis, hearing loss, loss of taste in half the tongue, ear pain, and skin lesions near the ear and ear canal.
Diagnosis and Treatment
A diagnosis of oral herpes is usually made following a visual examination by a doctor, though swab culture testing or blood tests may be performed to confirm the presence of HSV-1.
As the symptoms of genital herpes are variable, people with a lesion of any kind (blister, ulcer or sore) should see a medical professional for testing. A diagnosis of genital herpes is usually made following a visual examination, but swab testing may be conducted to confirm the diagnosis. Laboratory tests include microscopic examination and blood tests for antibodies to HSV-2.
Diagnosis of herpes zoster can be difficult before the blisters appear, but the sensation of pain in a band on one side of the body can be a clue. However, an accurate diagnosis typically follows the appearance of a rash combined with knowledge of a previous case of chickenpox or shingles. Testing is not usually needed but may include tests on blood or blister fluid.
There is no cure for either type of herpes infection at this time. However, a vaccine that may prevent herpes zoster has been approved. However, vaccines cannot treat shingles or post-herpetic neuralgia once they have started.
Although there is no cure for the virus, the symptoms of herpes can be treated.
Many patients with oral herpes choose not to treat cold sores unless the outbreaks are severe or frequent. Patients with genital herpes are more likely to undergo treatment. Three oral anti-viral medicines are approved for treatment of genital herpes:
- Acyclovir
- Famciclovir
- Valacyclovir
The drugs work by attacking the virus and disrupting its ability to multiply. All are safe to use; nausea and headache are the most common short-term side effects. No long-term side effects have been reported. Antiviral drugs are commonly prescribed for patients to treat primary infections, but they can also be used for recurrent infections. One of the drugs, valacyclovir, has been shown to reduce the risk of transmitting the virus to a partner.
Two kinds of treatment regimens are prescribed:
- Episodic therapy: Medication is taken at the first sign (even during the “warning symptoms” phase) of a recurrent outbreak and continued for several days. This speeds healing and may prevent an outbreak from being fully expressed. Some evidence indicates that there may be little benefit to taking the medication once lesions have appeared.
- Suppressive therapy: There are no approved oral anti-viral medications for oral herpes. For patients with frequent or severe outbreaks, some physicians will prescribe the oral anti-viral drugs approved for genital herpes. Two topical anti-viral medications (aciclovir ointment and penciclovir cream) are available by prescription to speed up healing of lesions and reduce viral shedding. Over-the-counter creams are also available, but only one, containing docosanol, has been approved and proven to speed healing.
Herpes zoster often disappears on its own. Treatment is usually directed at symptom relief with the following types of medications:
- Antiviral medications: If herpes zoster is diagnosed early, acyclovir or other antiviral medications may be prescribed to shorten the duration of the illness, minimize pain and reduce the chances of complications. Antiviral medications may also help those patients with compromised immunity or severe cases of shingles. Antivirals work best when started within 24–72 hours after the pain begins.
- Corticosteroids: Corticosteroids such as prednisone can reduce inflammation and lower the risk that post-herpetic neuralgia may develop, particularly in elderly patients. Corticosteroids are prescribed cautiously and seldom due to possible adverse effects.
- Analgesics (pain relievers): Mild pain may be controlled with over-the-counter medicines containing acetaminophen or ibuprofen. If pain is severe, a doctor may prescribe stronger medication.
- Antihistamines:Itching may be relieved by applying antihistamine creams or lotions topically (directly to the body) or taking antihistamine preparations orally (by mouth).
Natural treatments: A variety are available:
- Creams containing capsaicin (extracted from peppers) may help prevent post-herpetic neuralgia.
- Cold, wet compresses reduce pain.
- Oatmeal baths, starch baths and calamine lotion ease itching and discomfort.
In addition, researchers are exploring new methods for treatment for the herpes viruses and their complications. For example, the National Institute of Neurological Disorders and Stroke (NINDS) conducts shingles research. As well, new drugs and treatments may be tested now through clinical trials across Canada. To learn more about possible new treatments, visit our clinical trials page
Footnotes
*All information on medical treatments on this site is provided as an overview only. For a complete and up-to-date list of side effects, warnings and precautions, read the product’s package insert and consult your doctor or a pharmacist.
**If you are considering an alternative or complementary therapy, discuss it with your doctor first, and always be sure to keep your doctor up to date about any vitamins, supplements, or other forms of alternative treatment you are taking. Like any medication, alternative therapies can interact with other medications/treatments and, in some cases, have side effects of their own. Remember that “natural” does not necessarily mean “safe.”