Resources
If you are living with Skin Cancer, or know someone who is, you may want to stay up-to-date on the condition as well as current treatments and news.
Our Affiliate Members:
![]()
Canadian Skin Cancer Foundation
Other Resources
If you are living with Skin Cancer, or know someone who is, you may want to stay up-to-date on the condition as well as current treatments and news.
![]()
Canadian Skin Cancer Foundation
The information in this section has been gathered from existing peer-reviewed and other literature and has been reviewed by expert dermatologists on the CSPA Medical Advisory Board.
Skin cancer results from cells that multiply out of control. As a result, tumours, lumps, or masses can sometimes form on normal skin, and can be either benign (non-cancerous) or malignant (cancerous). Skin cancers are generally categorized as non-melanoma skin cancers (basal cell and squamous cell cancers) and melanoma.
There are three main types of skin cancer found in the outermost layer of skin, the epidermis:
The difference among the three is the type of cells that the cancer affects. In the case of non-melanoma skin cancers (i.e., basal cell carcinoma and squamous cell carcinoma), the cell affected is the keratinocyte. In human skin, this cell starts out at the basal layer (the lowest layer of the epidermis) and then moves up to the squamous (or middle ) layer of our skin. The non-melanoma cancers derive their names from where in the epidermis the affected keratinocyte is located.
Keratinocytes are the most common cell in the epidermis, the outermost layer of skin. These cells produce keratin, a tough, highly fibrous protein that acts as a barrier in our skin to provide waterproofing and prevent injury and invasion from microbes. This protein is also found in our hair, nails and tooth enamel.
You are more likely to develop a non-melanoma cancer if you have a family history of skin cancer, have already had skin cancer, or have fair or freckled skin, blue eyes and light-coloured or reddish hair. However, anyone who has had excessive sun exposure, severe and frequent sunburns during childhood, or lives in a sunny or high-altitude climate is at increased risk of developing skin cancer. Those who use immunosuppression drugs following an organ transplant, and other patients with suppressed or weakened immune systems are also at higher risk of non-melanoma cancer.
Although you can’t change some of these risk factors, some ways to reduce your risk include decreasing sun exposure, using sunscreen or long-sleeved clothing, avoiding sunburns, having regular skin check-ups, and avoiding tanning lamps and beds.
Looking Deeper
One of the primary causes of the DNA damage that leads to skin cancer is exposure to ultraviolet (UV) radiation from the sun and tanning lamps. However, genetic predisposition also plays a part. In fact, researchers have identified several genes that are linked to skin cancer. The "patched" (PTCH) gene often changes in basal cell carcinomas, while the p53 gene sometimes mutates in squamous cell cancers. While likely not the only genes associated with these carcinomas, they do give researchers some new clues in understanding these diseases.
Causes
Basal cell carcinoma: Most basal cell carcinomas are caused by exposing unprotected skin to the ultraviolet (UV) radiation in sunlight. The UV radiation damages genes that regulate cell growth and division. One gene commonly found to mutate (change) in basal cell cancers is the “patched” (PTCH) gene. Changes in this tumour-suppressor gene, which normally helps keep cell growth in check, can allow cells to grow uncontrollably. PTCH is unlikely to be the only gene that plays a role in the development of this skin cancer. Researchers are still working to fully understand the cause.
Nevoid basal cell carcinoma syndrome: This rare genetic condition is also known as Gorlin syndrome, or basal cell nevus syndrome. It is characterized by numerous basal cell carcinomas of the skin as well as jaw cysts seen on xray, palmar and plantar pits, calcified folds of the brain seen by radiography, hamartomas, various noncancerous growths, and skeletal anomalies affecting the ribs, hands and face. Annual magnetic resonance imaging (MRI) for infants and children with the syndrome for medulloblastoma screening should be performed until the age of eight years.
Squamous cell carcinomas: Most squamous cell carcinoma is caused by exposure of unprotected skin to ultraviolet (UV) radiation. Repeated, unprotected exposure to UV light, especially in the few years previous to diagnosis, increases the risk of developing squamous cell carcinoma. The UV radiation damages genes that regulate cell growth and division. People with weak immune systems are also at greater risk of developing squamous cell cancers. The gene commonly found to mutate in squamous cell cancers is called p53. Changes in this gene, which normally causes cells to die, may cause abnormal cells to live longer and perhaps become cancerous. Gene p53 is unlikely to be the only factor in the development of skin cancer. Researchers are still working to fully understand the cause.
Actinic keratosis (AK): This condition consists of one or more pre-cancerous skin lesions (pre-malignant). Thought not a cancer, some researchers believe it is an early form of squamous cell carcinoma. Only a small percentage of actinic keratoses go on to become squamous cell carcinoma. The lesions are strongly associated with UV exposure and sun damage. (The words literally mean “sun-induced rough spots.”) Risk factors include being over the age of 40, exposure to high levels of UV radiation, and a weak immune system.
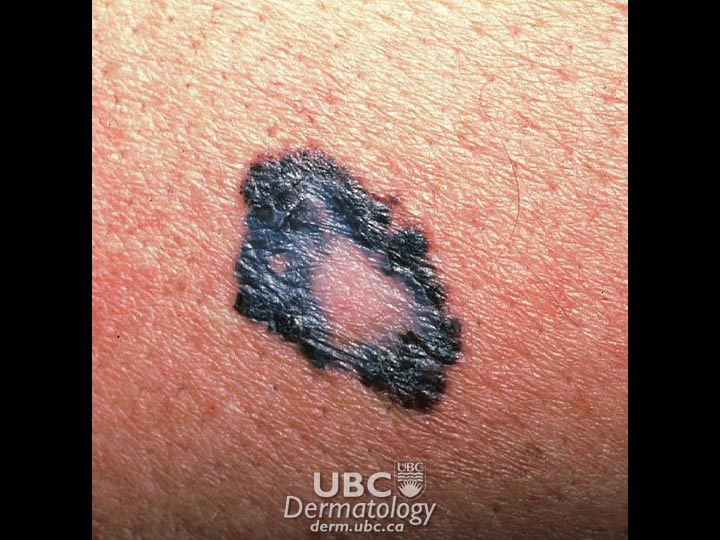 Melanoma
Melanoma  Basal Cell Carcinoma
Basal Cell Carcinoma  Squamous Cell Carcinoma
Squamous Cell Carcinoma  Melanoma
Melanoma
Fast Facts
The most common sign of skin cancer is a local change in the skin’s colour or a sore that does not heal. However, skin cancer symptoms vary widely according to type, so it’s wise to check your skin regularly to catch any potentially cancerous marks early.
This type of cancer begins in the lowest layer of the epidermis (the basal cell layer), usually on sun-exposed areas, such as the head, neck, and upper shoulders. However, 20% of people with basal cell carcinoma develop it in areas not exposed to the sun. This type of cancer grows slowly and rarely spreads to other parts of the body, but if left untreated, it will continue to grow and may ultimately invade the bone or other tissues beneath the skin. Basal cell carcinoma is usually treated successfully as an out-patient procedure. Symptoms include:
Skin growths are similar to basal cell carcinomas. In addition, the person may also have:
This carcinoma begins in the upper layer of the epidermis (squamous cell layer), usually on sun-exposed areas, such as the head, neck and back of the hands. However, it may appear on skin elsewhere on the body (such as the lips, tongue or the lining of the mouth) and on skin that has been burned or exposed to chemicals or radiation therapy. Of these tumours, 95 per cent can be cured if found and treated early, particularly if they arise in areas of sun-damaged skin. Rarely, squamous cell carcinomas can grow and spread to lymph nodes. Symptoms include:
Bowen’s disease isatype of squamous cell carcinoma limited to the epidermis. The affected area is red-brown and scaly or crusted and flat. It may resemble a patch of dermatitis, psoriasis, a fungal infection or a type of basal cell carcinoma.
These spots can look like regular skin, but may feel like sandpaper. Symptoms and signs include:
To diagnose non-melanoma carcinomas, a doctor will take your medical history and perform a physical exam. If cancer is suspected, your doctor may take a skin biopsy, which will be used to confirm the diagnosis. A biopsy can be taken in one of four ways:
A biopsy can be done in the doctor’s office or in a hospital’s outpatient department. It requires a local anesthetic and sometimes stitches, depending on how much skin is removed. The tissue sample will then be checked with a microscope to determine the diagnosis. .
Generally, the earlier non-melanoma skin cancers are caught, the more successfully they can be treated. Visit your doctor if you develop a new skin lesion that does not heal, notice a change in a pre-existing skin lesion (such as a mole), or have any of the symptoms or signs of non-melanoma carcinoma.
Basal cell carcinoma treatments include the following:
Nevoid basal cell carcinoma syndrome can be treated through:
Squamous cell carcinoma treatments include:
Actinic keratosis treatments involve:
In addition to the treatments above, Canadian researchers are continually exploring new ways to treat non-melanoma skin cancers. Some may be conducting research studies known as clinical trials, which test new medications and treatments that are being developed. To learn about new research on all types of non-melanoma cancers happening in Canada, visit the clinical trials section [link to clinical trials section].
Footnote
*All information on medical treatments on this site is provided as an overview only. For a complete and up-to-date list of side effects, warnings and precautions, read the product’s package insert and consult your doctor or a pharmacist.
**If you are considering an alternative or complementary therapy, discuss it with your doctor first, and always be sure to keep your doctor up to date about any vitamins, supplements, or otherAlthough a cancer diagnosis is never welcome news, basal cell carcinomas are usually easily curable. With such high success rates, they usually do not negatively impact a person’s everyday life. However, patients may feel anxious knowing that their cancer may return, or may feel depressed if surgical removal of larger tumours leaves a scar or causes extensive damage to underlying tissues or bone.
Most squamous cell carcinomas are also easily treated and generally do not affect a person’s quality of life. In rare instances, people with this disease may suffer emotional trauma if their cancer progresses and requires long-term treatment or becomes life-threatening.
Non-melanoma skin cancers are curable most of the time, especially if caught early. With this, gentle reassurance alone is often sufficient to help someone successfully manage their fears. However, people with skin cancer who experience anxiety, depression or stress may seek professional counselling to manage their feelings or seek support from others who understand their situation.
Charitable Number: 80425 7814 RR 0001