 |
|
|
|
|
 |
|
Clinical Trials Brochure
|
|
|
|
|
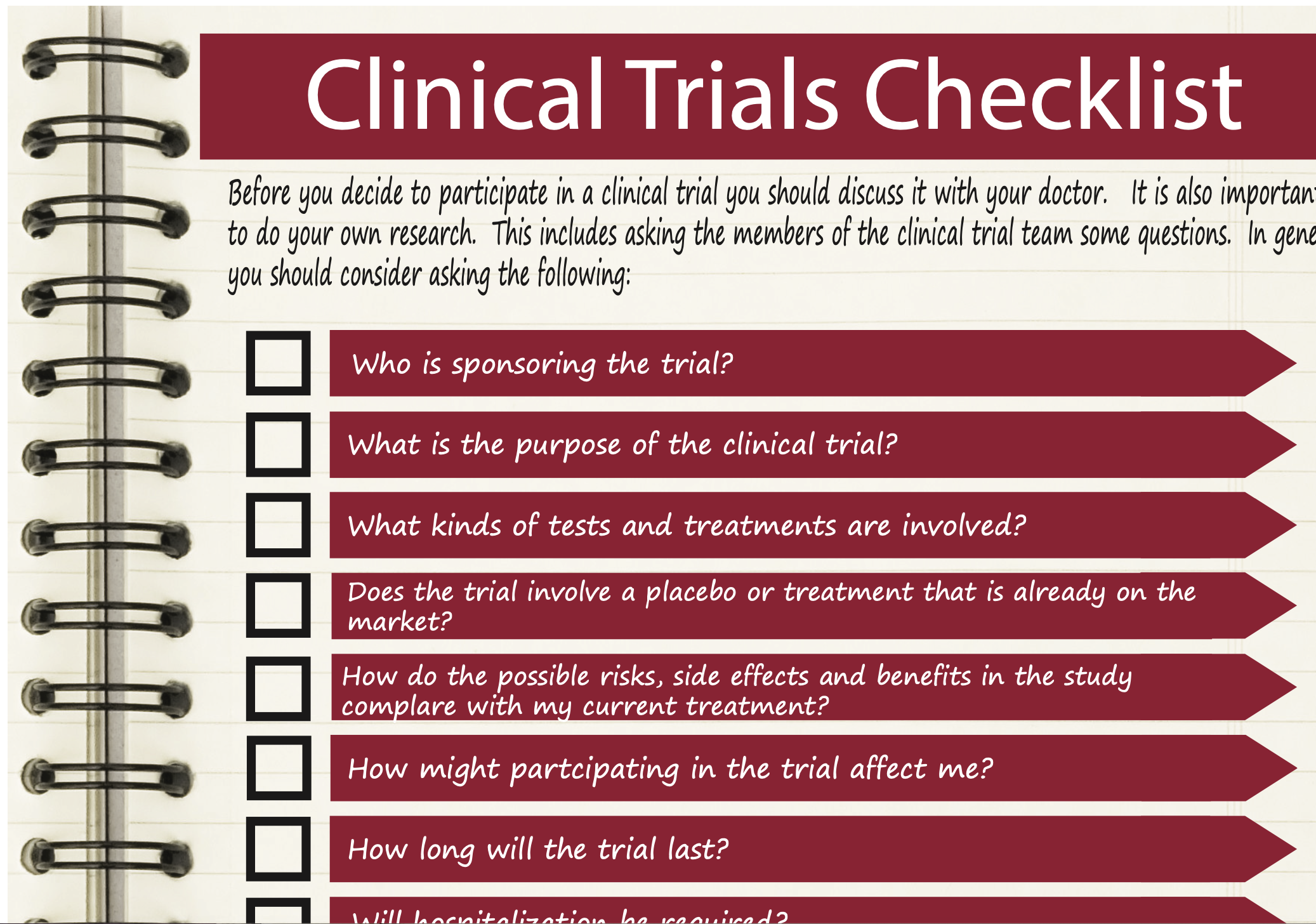
Clinical Trials Checklist
|
|
What is a clinical trial?
A clinical trial is a research study that attempts to answer specific health questions by working with human volunteers. There are two primary kinds of clinical trials:
• Intervention trials are used to test a new treatment to slow down a condition or manage its symptoms more effectively.
• Observational trials are used to attempt to learn more about a health condition.
Clinical trials are very carefully planned, coordinated, and monitored. By working with human volunteers, they give scientists their best opportunity to evaluate potential therapeutics and medicines by studying their effects on both healthy people and those living with the condition they are meant to address.
Clinical trial doctors/ researchers are also called clinical trial/ study investigators in the clinical trial setting. The researchers are suitably qualified and make attestations as required by Health Canada, in order to conduct the clinical trials in Canada.
Why participate in a clinical trial?
There are a number of reasons why someone would participate in a clinical trial, such as:
1. Clinical trial participants are among the first people to receive potential new treatments for a condition;
2. Participation in a clinical trial allows people to make a valuable contribution to research;
3. Clinical trial participation allows a person to play a more active role in his or her health care; and
4. Involvement in a clinical trial can give a person greater access to a team of experts who may be able to provide deeper insight into his or her condition.
What are the risks of participating in a clinical trial?
While clinical trials are closely monitored and planned, they do involve risks:
1. There may be side effects to the treatment, ranging from minor or unpleasant side effects to more serious ones that require medical attention.
2. The treatment may not be effective for some participants.
3. Some participants may experience discomfort related to the additional medical tests and procedures.
Joining a clinical trial may require some participants to interrupt the treatment they were receiving before joining the clinical trial.
Who is eligible to join a clinical trial? How will I know if I am eligible?
Each clinical trial has its own criteria about who can participate in it. There are two types of criteria:
• Inclusion criteria, which determine if someone is eligible to participate in the trial.
• Exclusion criteria, which determine if someone is not eligible from participating.
These criteria are very carefully considered by the researchers and scientists when designing the trial. They are important parts of the clinical trial itself, as they allow researchers to control the variables of the trial to better the quality of the data and results of the study. That is why, even though you may have the medical condition being studied, it may be determined that you are not suitable for the particular trial
Some potential inclusion and exclusion criteria include the following:
• age
• gender
• stage or severity of a disease
• previous treatments taken (or not taken) by a patient
• current medication
• medical conditions other than the one being studied.
• Participation in other studies
Ultimately, the clinical trial staff will inform you if you are eligible or not.
What are my rights as a participant?
Clinical trials—and the treatment of participants in those trials—are highly regulated. In addition to being subject to a series of independent reviews and measures, Canadian clinical trials are regulated by Health Canada (the federal government), which in addition to Canadian specific requirements bases its regulations on a set of international standards called Good Clinical Practices (GCP) which were developed and agreed by global authorities at the International Conference on Harmonisation (ICH).
Those regulations entitle participants to a number of important rights.
Confidentiality and privacy
Once you are deemed eligible for the trial and have given your consent, your personal health information will be collected during the trial, including items such as physical examination details, test results, imaging results, blood tests, and tissue samples. Trial staff also will have access to your original medical record.
Activities related to your personal information are regulated by the Personal Information Protection and Electronics Documents Act (PIPEDA), which is part of the Canadian Privacy Law. PIPEDA requires participant consent for collecting personal and identifiable information. It also requires trial staff to inform participants of their privacy rights and to provide them with the opportunity to learn about what information is being collected and why.
Information from the trial will be submitted to the trial sponsor (see below), Health Canada and possibly government agencies from other countries (such as the US Food and Drug Administration, FDA), but that data remains anonymous. Even if results are published in scientific journals, no personal information is released: the data is valuable because it represents results accumulated from many participants in aggregate, and not specific individuals.
Overall, your information will be kept in a secure location and only viewed by select members of the clinical trial (such as the trial doctor, staff helping the trial doctor, representatives from the sponsor, and the Ethics Committee).
Access to your own data
As a clinical trial participant, you have the right to see your trial records. Depending on the trial, however, you may not be able to review or make a copy of your records until the study has concluded: sharing trial data with anyone outside of the study before it is complete might compromise the confidentiality and integrity of the trial.
Withdrawal at any time
Clinical trial participants have the right to leave a trial at any time. Data collected from participants prior to their withdrawal will still be used by the researchers.
If you do stop your participation, you should inform the research team know about it and tell them your reasons for leaving. They may want you to return for a final evaluation or tests.
Best possible care
Clinical trial doctors are responsible for providing you with the best possible medical care throughout the study. Depending on the protocol (a document that describes the design and methodology of the trial), they also will provide the same level of medical care and follow-up for an appropriate period once the study is complete.
Even if you withdraw from the trial early, you will continue to receive care for an adequate period.
It is important to note that clinical trial doctors do not replace your everyday health care professionals. In fact, if you give them permission, trial doctors and your health care team may collaborate to share information and avoid repeating tests.
Informed consent
Informed consent is a crucial part of the clinical trial process. Mandated by law (see “Confidentiality and privacy,” above), informed consent is an ongoing process that ensures anyone who wishes to participate in a trial fully understands the study and its objectives.
- Before the trial, potential participants learn about the trial, including its purpose, duration, procedures and other details. The risks and benefits also should be explained at this stage. If the person still wishes to participate after being provided with this information, they can then sign the informed consent document.
- During the trial, participants will be informed of any new information that may affect their continued participation in the trial.
It is important to remember that the informed consent document is not a contract: it is to protect your rights at all times. You can still withdraw from the trial at any time (see “Withdrawal at any time,” above).
What are my responsibilities a patient?
As a participant in a clinical trial, you have several responsibilities, which will be outlined in greater detail in the informed consent form.
- You must inform the clinical trial team about any past or current medical conditions or allergies. You also report any side effects or changes in your condition to the clinical trial team, particularly if you choose to withdraw from the study.
- You should be prepared to remain in the trial for its duration. You can, of course, withdraw at any time (see “Withdrawal at any time,” above), but it is important for the integrity of the study to stay until the trial is complete, if you can.
- You may be required to cover some indirect costs (see “What are the potential expenses?” below).
Perhaps your greatest responsibility is to read and understand the informed consent form and to remain an active participant in the trial.
Who are the important parties?
Clinical trials not only involve a team of health professionals, but also a collection of other people and organizations that oversee its operation and management. The following are a few of the important parties that you may encounter during your participation in a clinical trial.
Sponsor
The sponsor is the group or organization that initiates the trial. It can be a pharmaceutical or medical device company, a university, a health-care institution, a voluntary group, a government body, or an individual physician or care provider.
Ethics Committee
An Ethics Committee is comprised of physicians, researchers and community members. Its role is to review, approve, and monitor a trial: before any clinical trial can begin in Canada, its principal investigator must present a detailed request to the Ethics Committee that has been tasked with reviewing the trial. Ethics Committees also periodically review trials to protect the rights of participants.
Ethics Committees also can be called an Ethical Review Board, an Independent Ethics Committee, an Institutional Review Board (IRB), or a Research Ethics Board (REB).
Clinical research coordinator
The clinical research coordinator (or study coordinator) handles the day-to-day logistics and reporting of the trial. Often a certified nurse, the study coordinator frequently is involved in the informed consent process and ensuring compliance with the trial protocol. The coordinator also makes sure that the trial visits, tests and procedures are scheduled on time, and that patients understand how to take the study drug and complete the trial questionnaires or diaries.
Investigator/principal investigator
The investigator or principal investigator (often called the “trial doctor”) is the highly trained doctor who carries out the research and interacts with the patients. Investigators have completed additional training on conducting clinical trials and research, with particular emphasis on trial patients.
The principal investigator is in charge of how the trial is conducted, and he or she supervises the team of trial professionals who contribute to patient safety
What are the potential expenses? Will they be reimbursed?
Any treatment received as part of most clinical trials is provided free of charge. The only exception is in Phase IV observational trials, when the drug has already been approved by Health Canada. In those instances, the cost of medication is the responsibility of the patient, although there are insurance and other support programs that may provide reimbursement.
There are some indirect expenses that clinical trial participants may need to pay on their own:
- travel costs to and from the clinic or research site (although some trials will reimburse you for these costs)
- babysitting or childcare
- household help (if you have less time to perform chores)
- lost income (if any).
The trial coordinator can help you determine your costs over the full trial period and whether or not any will be reimbursed.
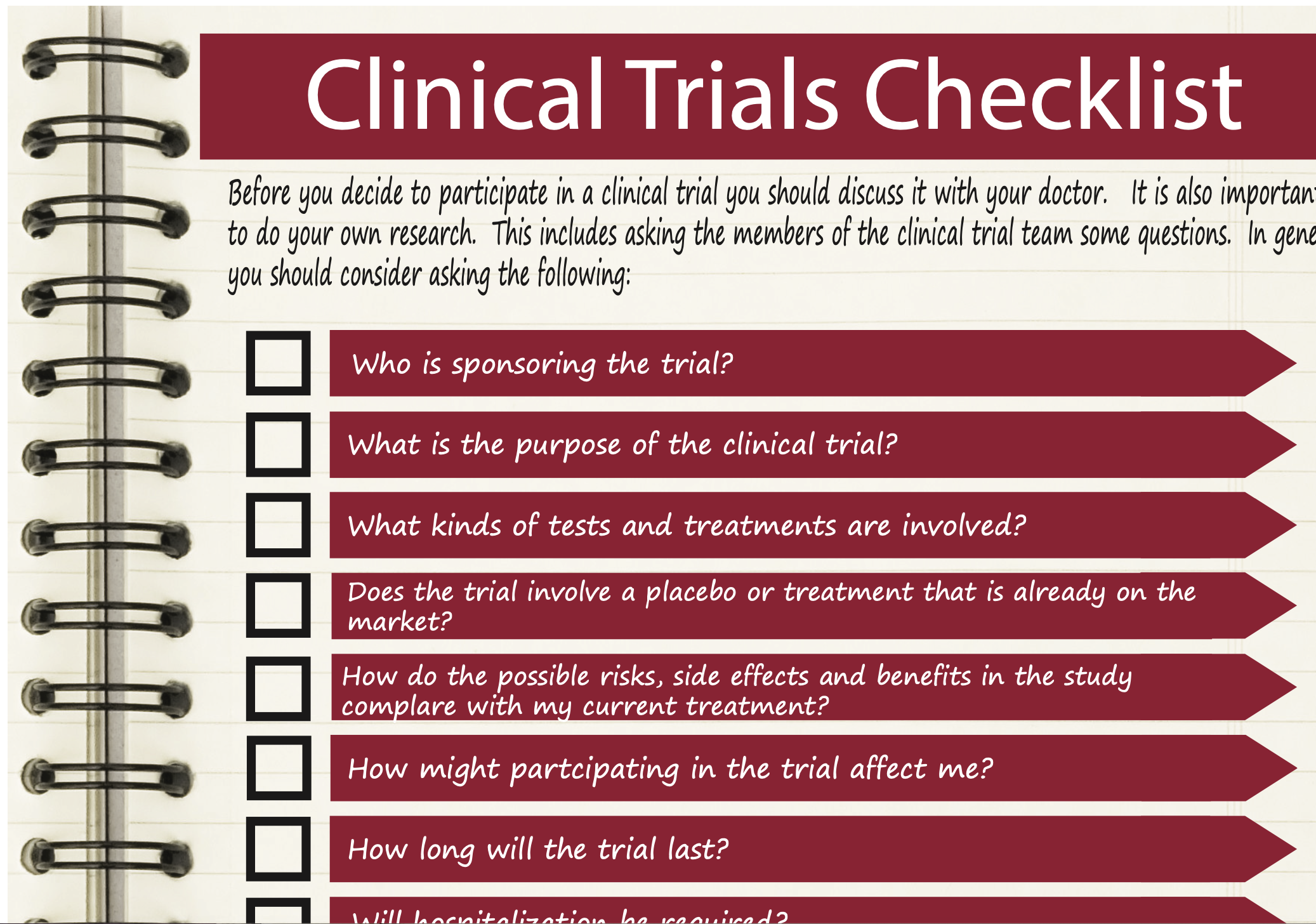
What should I consider before participating in a trial?
Before you decide to participate in a clinical trial, you should discuss it with your doctor. He or she will tell you if there are any medical reasons for you not to participate in the trial.
It also is important for you to do your own research. This includes asking the members of the clinical trial team some questions.
In general, you should consider asking the following:
- What is the purpose of the clinical trial?
- Who is sponsoring the trial?
- What kinds of tests and treatments are involved?
- Does the trial involve a placebo or treatment that is already on the market?
- How do the possible risks, side effects, and benefits in the study compare with my current treatment?
- How might participating in the trial affect me?
- How long will the trial last?
- Will hospitalization be required?
- Who will pay for the treatment? Will I be reimbursed for other expenses?
- What type of follow-up care is part of the study?
- Will results of the trial be provided to me?
- Who will be in charge of my care? Will I be able to see my own doctor?
- Can I keep using the treatment after the study if it works for me?
- What privacy and confidentiality precautions are being taken with personal information?
You can find a helpful printable and mobile-friendly list of potential questions here.
You should also discuss the trial with family and close friends. Ask them to help you with the research and decision-making process: this will help them to provide better support for you should you decide to join the trial. A friend or family member also can attend your meeting with clinical trial staff to discuss your potential participation.
Do I have to tell my employer or co-workers that I am participating in a clinical trial?
It is up to you to decide who you tell about your involvement in a clinical trial. You are not legally required, however, to inform your employer: if you need to take time off for the trial, you can decide to use vacation days to cover that time.
If you do decide to tell your colleagues about your involvement in a trial, there is no need to go into great or personal detail. You can simply tell them you are participating in research and provide a brief overview of why you have decided to do so. Again, the decision of whether or not to tell them—and how much—is up to you.
How do I find out about clinical trials?
It can be a challenge to find a clinical trial that is relevant for you. Your doctor may direct you to a promising trial, but you also can search databases and websites dedicated to clinical trials. You can find some of these websites under “Additional resources” (below). In particular, you will want to visit the Patients at Heart, Clinicaltrials.gov and Canadatrials.com sites, all of which provide some clinical trial listings (as well as other resources).
Make sure that the sources you search are reputable ones! If you find a trial on a site that is not listed below, be sure to research it thoroughly to ensure that the trial is a legitimate one. If you have any doubts at all, be sure to check with your doctor and ensure that it is registered on the Clinicaltrials.gov website.
Additional resources
CSPA Clinical Trials Brochure - printable pdf
Clinical Trials Ontario: COVID-19 Resources and updates (
ctonario.ca)
This site contains resources about clinical trials to learn more about the impacts of COVID-19, with a comprehensive list of clinical trials taking place in Ontario.
Canada Trials (canadatrials.com)
CanadaTrials.com contains a searchable database of clinical research trials that are actively enrolling patients in Canada. It also provides general health information and links to patient support programs.
The Center for Information & Study on Clinical Research Participation (CISCRP)(ciscrp.org)
CISCRP is a nonprofit organization in the United States that works to educate and inform the public, patients, lawmakers and medical community about clinical research. Their site is an excellent source of information about clinical trials for patients, although some of the resources are specific to the medical system in the United States.
CenterWatch (centerwatch.com)
CenterWatch is an unbiased source of information on clinical trials. It also includes a database of clinical trials that can be searched by condition, therapeutic area or location.
ClinicalTrials.gov (clinicaltrials.gov)
Part of the U.S. National Institutes of Health (NIH), ClinicalTrials.gov provides a registry and database of clinical trials from around the world. It is the gold standard when it comes to listings of clinical trials: most legitimate trials are registered on its database. It is worth noting that the database here is quite complex and not always user-friendly. The site does provide a selection of resources for patients and their families, however, including instructions on how to use the database.
Health Canada (hc-sc.gc.ca) http://www.hc-sc.gc.ca/hl-vs/iyh-vsv/med/clinical_trials-essais_cliniques-eng.php#a2
Health Canada is the government department responsible for “helping Canadians maintain and improve their health.” Their homepage contains the latest health updates and health-related information.
International Conference on Harmonisation (ICH)(ichgcp.net)
The ICH is the international body that outlines Good Clinical Practice, which is the “standard for the design, conduct, performance, monitoring, auditing, recording, analyses, and reporting of clinical trials…”.
Network of Networks (N2)(n2canada.ca)
N2 is “not-for-profit…alliance of Canadian research networks and organizations working to enhance national clinical research capability and capacity.” Their “Resources” page contains a selection of resources about clinical trials.